Is the current number of testing conducted enough? This is always a concern for the medical community and general public alike. The simple and no brainer answer to that question is – there is never enough testing. The best number of testing, in an ideal situation, is to get each and every single person tested. By doing so, we can be absolutely sure of the exact number of people who are positive for COVID-19.
So, what is the next best number for testing the masses? The answer is “as many as possible”. The closer it is to 100%, the better. With a bigger number of people tested, we are more confident and surer that the figure is almost as close to the actual number if the testing was done onto everyone.
However, it is not as simple as that. The practical application of widespread testing varies in different locations, for example, between Kuala Lumpur and Kapit. For testing to be efficient, it has to be tailored according to the different demographics, disease pattern and social circumstances of each.
Performing widespread testing in the community has its own caveat. Massive testing is known to be resource-depleting. Manpower and money are limited. In an epidemic of an unknown and new disease, the surge capacity of many facilities might be limited in the initial phase and this includes the availability of capable laboratories. As seen in Malaysia, the initial 6 laboratories that were used for COVID-19 testing were inadequate to withstand the surge in demand for increased testing needs. This capacity was increased to 43, with the inclusion of laboratories from various health institutes and universities.
The very rapid spread of an infectious disease in the community demands a targeted testing approach. Blind massive testing may result in a missed opportunity to initiate early control or prevention activities in a specific community. Hence, a strategy is needed to bypass these limitations. Being selective may be the key to efficient testing.
Testing High Risk Groups
However, being selective in testing is not risk-free. Wrongly selecting the group of people to be tested could be disastrous. The question is, how do we pick out the enemy hidden among the masses? A proper tool is needed to avoid a guessing game. Otherwise, there are chances that blind spots -will result in hotspots and become a continuous source of infection to the community.
Therefore, recent data which is up-to-date is needed to determine who to test. The challenge is to what degree can we trust the available data as these data only emerge recently, in the wake of a new outbreak. Traditionally, outbreaks of known infectious diseases provide historical understanding that allows iteration of the data. With the advancement of machine learning and artificial intelligence, the complex iteration provides guides with high precision on who to target within the community.
There are many ways that we can use the information to prioritise testing in the population. We might want to consider people who might be worse off if they contract COVID-19. These include the elderly and those with chronic illness – such as diabetes and hypertension. Next on the list are those who are likely to be in contact with potential cases – the health care workers, the defence personnel and even teachers. People who are institutionalised, living in close quarters such as prison inmates and nursing homes are also considered, as they run a high risk of infection.
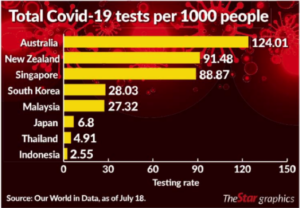
Image source: star.online
We should not look within our country only. We need to look over our borders and be more concerned particularly with those countries who we share our borders with. What is their current incidence of reported cases? If the number is low, what about their testing rates? Looking at the recent data, at the time of writing, Singapore still records three digits daily, recording new cases at the rate of 821 cases per 100 000 people, Indonesia records 32.25 of new cases per 100 000 people, Brunei 32.23 new cases per 100 000 people, and Thailand 4.66 per 100 000 people.
However, one may be slightly reserved with the rate of new cases reported after looking at the testing rate. While Malaysia and Singapore record a relatively high testing rate compared to the other ASEAN countries, with 27.7 and 88.9 tests per 1000 population respectively, we should be concerned with other neighbouring countries such as Indonesia. Indonesia, a populous country with 273 million people, and shares a huge chunk of its border with Malaysia only has a testing rate of 2.63 per 1000 people. The Philippines is another populous country neighbouring Malaysia with 109 million people records a testing rate of 9.94 per 1000 people. The numbers seem small, given the population size and the rate of positive cases. However, the benefit of doubt should be given to them, looking at their expanse and geographical make up.
But is that acceptable?
One factor that needs to be considered for adequate testing is the size of the outbreak. The bigger the outbreak, the more testing is needed (7). However, the only way to know the size of the outbreak is by testing. By knowing the number of infected people, prediction models could be constructed by data modellers. The models can be referred to, in deciding the adequacy of the testing.
Another method to determine if a country adequately tests for COVID-19 is to look at the positivity rate – i.e. the percentage of tests that come back positive. However, caution needs to be applied when interpreting the positive rates.
Very high positive rates could mean that a country has tested its population-wide enough to find the cases (2). However, it could also mean that the country may have only tested the sick patients seeking treatments in health centres (data would usually be collected from these places) and not casting their nets wide enough to determine the spread of the disease in the community (3). Or it could also indicate a true increase in disease transmission (4).
The number is not an absolute number to fall back on in prescribing the next course of action. However, the WHO has made an ad hoc recommendation that the positivity rate should be below 10% to reflect adequate testing. Anything more than 10% means that testing is not sufficient to detect undetected cases in the community. In April 2020, Malaysia’s positive rate stood at 5% (6), which was viewed as adequate. According to the WHO again, for a country to re-open, or relax in its restriction, positive rates should be below 5% for at least 14 days.
Is testing important?
Yes, testing is important as a guide to gauge the preventive activities that we have done thus far. Of course, just looking at the testing ability is narrow in scope. In some places, more testing has resulted in back log in reporting positive cases, painting a delayed view of the current scenario. A delay in informing a result leads to further disease spread, longer quarantine time that leads to higher expenses and prolonging of the outbreak.
Conclusion
The outbreak is not going to end that soon. There is a promising light at the end of the tunnel. We are currently dealing with a few missteps – careless individuals who defy quarantine orders and those who do not take the prescribed Standard Operating Procedures (SOPs) seriously. To the administrator, a middle ground is needed between the adequacy of testing and cost that the testing incurs. To the rakyat, the perceived inadequacy of testing is a concern. The truth is, testing will never be enough. But, like a double-edged sword, testing could prove beneficial or otherwise. It is the smart use of testing that is needed.
Reference:
- https://theconversation.com/how-much-coronavirus-testing-is-enough-states-could-learn-from-retailers-as-they-ramp-up-136494
- https://ourworldindata.org/coronavirus-testing#the-positive-rate-are-countries-testing-enough-to-monitor-their-outbreak
- https://coronavirus.jhu.edu/testing/testing-positivity
- https://www.medscape.com/viewarticle/933892?nlid=136498_440&src=WNL_mdplsfeat_200721_mscpedit_publ&uac=23693HZ&spon=42&impID=2470660&faf=1
- https://www.statnews.com/2020/04/27/coronavirus-many-states-short-of-testing-levels-needed-for-safe-reopening/
- https://codeblue.galencentre.org/2020/04/19/malaysia-tested-109000-people-5pc-positivity-rate-enough-moh/
- https://www.npr.org/sections/health-shots/2020/05/07/851610771/u-s-coronavirus-testing-still-falls-short-hows-your-state-doing
- https://www.nytimes.com/interactive/2020/us/coronavirus-testing.html?auth=login-google1tap&login=google1tap
- https://www.europeanpharmaceuticalreview.com/article/125084/the-malaysian-response-to-covid-19-building-preparedness-for-surge-capacity-testing-efficiency-and-containment/
