 As of 30th of May, more than 300 confirmed or suspected cases of Monkeypox have emerged in over 20 countries. Since the outbreak was first reported in the UK, the virus began to be detected across Europe – with public health agencies in countries like Spain, Germany, France, the Netherlands, Italy, and Sweden all confirming cases. The perplexing news is that these cases are reported from countries that are not endemic for Monkeypox virus. It has made headlines in several countries since the global surge of Monkeypox1. Many Malaysians, barely stepping out of the shadows of Covid-19, are fearful of yet another pandemic.
As of 30th of May, more than 300 confirmed or suspected cases of Monkeypox have emerged in over 20 countries. Since the outbreak was first reported in the UK, the virus began to be detected across Europe – with public health agencies in countries like Spain, Germany, France, the Netherlands, Italy, and Sweden all confirming cases. The perplexing news is that these cases are reported from countries that are not endemic for Monkeypox virus. It has made headlines in several countries since the global surge of Monkeypox1. Many Malaysians, barely stepping out of the shadows of Covid-19, are fearful of yet another pandemic.
The good news is that although Monkeypox is a potentially serious illness, it is still rare. In recent times, the case fatality ratio3 has been around 3-6% (although in some places, WHO reported fatality ratio of up to 11%). The disease spreads through close contact with an infected person or animals; or with material contaminated with the virus. Human-to-human transmission is via close contact with lesions, bodily fluids including respiratory droplets, and sexually transmitted and contaminated materials like blankets and towels.
The World Health Organisation (WHO) said the current Monkeypox outbreak outside Africa is ”unlikely” to lead to a pandemic. However, they emphasised that it still remains unclear if infected patients who are asymptomatic can transmit the disease. At present, there has been no cases reported in Malaysia and the risk of transmission is very low due to the limited human-to human transmission.
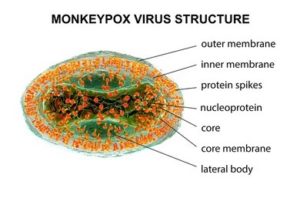 Monkeypox infection is caused by the Monkeypox virus, belonging to Orthopoxvirus genus in the family of Poxviridea. The Orthopoxvirus genus also includes variola virus (which causes smallpox), vaccinia virus (used in the smallpox vaccine), and cowpox virus. Monkeypox became the most prevalent orthopoxvirus after smallpox was eradicated in 1980. It is an uncommon zoonotic viral disease endemic to Central and West Africa. It is different from the Varicella-zoster virus (a herpes virus) which causes chicken pox.
Monkeypox infection is caused by the Monkeypox virus, belonging to Orthopoxvirus genus in the family of Poxviridea. The Orthopoxvirus genus also includes variola virus (which causes smallpox), vaccinia virus (used in the smallpox vaccine), and cowpox virus. Monkeypox became the most prevalent orthopoxvirus after smallpox was eradicated in 1980. It is an uncommon zoonotic viral disease endemic to Central and West Africa. It is different from the Varicella-zoster virus (a herpes virus) which causes chicken pox.
The first case of Monkeypox was reported in laboratory monkeys in 1950. Despite that, the main reservoir is rodents, contrary to the name Monkeypox. Other animal species that have been found to be infected with the virus include Gambian giant rats, striped mice, and squirrels.
However, the current Monkeypox outbreak is seeing a new pattern, where people with no direct connection with Africa are reporting cases. Many of these cases have been found among sexually active communities, especially those with lesions on their genitals and adjacent areas.
The incubation period of Monkeypox ranges from 6 to 14 days. The disease is often self-limiting within two to three weeks and patients normally find their symptoms resolving spontaneously. It typically begins with fever, headache, muscle ache and swelling of the lymph nodes, then progresses to rash on the face and body at day-3 of fever. Typically, the rash are seen around face (95%), palms & soles (75%), oral mucosa (70%), genitalia (30%) and conjunctivae & corneal (20%). The rash appears as macules, papules, vesicles, pustules and present at the same stage at any area. Unlike chicken pox, the vesicles of Monkeypox are usually larger than chickenpox2 and can be painful and monomorphic whereas chicken pox rash is usually polymorphic.
The presence of the lymph node enlargement before and concomitant with the appearance of the rash helps to point towards a diagnosis of Monkeypox rather than smallpox or varicella.
Institute for Medical Research (IMR) has the availability of laboratory tests for confirmation of monkeypox in Malaysia, which is by testing the vesicle/bodily fluids to identify with nucleic acids test by PCR or viral culture.
There is no specific treatment for Monkeypox, although the smallpox vaccine, cidofovir, ST-246, and vaccinia immune globulin (VIG) can be used to control a Monkeypox outbreak (by immunising close contacts). There are various reports that the smallpox vaccination offers 85% protection against Monkeypox infection, but these are not for active vaccination to general populations. It is also important to note that chicken pox (varicella) vaccine does not protect against the Monkeypox infection.
Most countries like Europe and Malaysia advocate self-isolation for 21 days for close contacts of Monkeypox patients. Asymptomatic close contacts should not donate blood, cells, tissue, organs, breast milk or semen while they are under symptom surveillance.
At present, there is no restriction for travelling to Monkeypox endemic countries. Nevertheless, it is advisable for travellers to be aware of updates regarding Monkeypox and avoid contact with sick, dead or live animals (rodents, marsupials, primates) that could be infected with the virus. They also should not eat or handle bush meat.
Additionally, travellers should always practice good self-hygiene including proper handwashing using soap and water. The use of alcohol-based sanitizers is strongly recommended when water and soap is not available. Travelers with any illness during travel or upon return should seek medical advice and be reported to health professionals. All probable or confirmed cases of Monkeypox must be notified to the nearest health district office within 24 hours.
Currently the risk to the public is said to be low, but with WHO expecting the cases of Monkeypox to rise, most countries are now increasing their surveillance. Our Ministry of Health has guidelines in place to handle Monkeypox and armed with accurate information, we will be able to curb the spread of the Monkeypox virus. As always, the public is urged to practice good personal hygiene and a healthy lifestyle to prevent any future infectious disease outbreaks.
By Dr Punithavathy Shanmuganathan, Senior Lecturer of Family Medicine and Dr Lim Yin Sear, Senior Lecturer of Paediatrics, School of Medicine, Faculty of Health & Medical Sciences, Taylor’s University
Bibliography
- Vasan A. NEW YORK CITY DEPARTMENT OF HEALTH AND MENTAL HYGIENE 2022 Health Advisory 6: CDC Advisory Monkeypox Virus Infection in the United States and Other Non-endemic Countries-2022 [Internet]. [cited 2022 May 23]. Available from: https://www1.nyc.gov/assets/doh/downloads/pdf/han/advisory/2022/cdc-monkeypox-us.pdf
- Health. Monkeypox [Internet]. Australian Government Department of Health. 2022. Available from: https://www.health.gov.au/health-topics/monkeypox
- World Health Organization: WHO. Monkeypox [Internet]. Who.int. World Health Organization: WHO; 2018. Available from: https://www.who.int/news-room/fact-sheets/detail/monkeypox
- About Monkeypox [Internet]. 2019. Available from: https://www.cdc.gov/poxvirus/monkeypox/about.html
