
Pic source: Working Mother
Every mother who has given birth will be able to relate the magical moment of breastfeeding her newborn. It is the moment when she feels fulfilled as a mother, and the immense joy of love as the baby sucks in every drop of the precious breast milk. The first few days after your baby is born, it is definitely the period of tremendous change of your life. You feed your baby every few hours, each time he or she demands for it. The “immense joy” may be replaced with an ‘overwhelming’ feeling in the next few days after birth: you could hardly rest or sleep as the baby cries to be fed every few hours, and even at night. At this time, these thoughts may cross your mind:
“I have “no milk” in the first week. I need to give the baby something to feed the baby”
“My baby cries too often. He is hungry. My breast milk is not enough for him”
“Why does he cry even after feeding as if he is not satisfied? Am I not producing enough milk for him?”

Pic source: BabyCenter
The above questions may linger in the mother’s mind more often than not especially in the first week after birth. Convinced with the perceived inadequate milk that she is producing, coupled with opinions or suggestions from visiting family and friends, or even some health care providers, the mother may decide to top up the baby’s feeding with formula milk instead. So that it will give herself peace of mind that she is making sure that her newborn baby is full and satisfied.
Does this seems familiar to you? Is it true that during the early days after giving birth, a mother needs to feed her baby with formula while waiting her breast milk to come in?
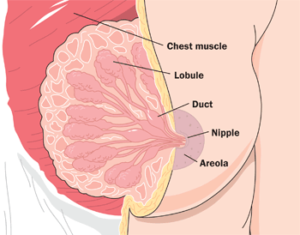
It is very important that every expecting mother understands the basics behind milk production, or lactogenesis before and after birth. Lactogenesis means the creation of milk. It is the process during which the mother actually starts producing milk which comes in stages. There are 3 stages which are lactogenesis I, lactogenesis II and lactogenesis III.
Lactogenesis 1
Pic source: WomanHealthGate
Your body will start producing milk around the middle (around 4 months or 16-22 weeks) of your pregnancy. This process is called lactogenesis 1. During this process, the cells in your breasts will swell up and starts to differentiate to milk producing cells. Some women may be able to express colostral fluid from this time, while others may see no sign of milk production until after the baby is born.
This fluid known as colostrum is a concentrated milk with high amount of antibodies and nutrients. During this period, your body is triggered to produce colostrum by hormones, which is called ‘hormones-controlled system’. Therefore, as long as your body is producing the right amount of hormones required to make milk, worry not, you are making milk! One of the hormones which is involved in this process is called progesterone. High levels of progesterone during the later part of pregnancy prevents milk secretion and keep the volume down. At this time, you will notice that your breast is slightly bigger than the pre-pregnancy state and visible veins are noticeable.
Lactogenesis II
Right after birth, after the placenta is delivered, the level of progesterone (as well as other hormones) drops suddenly. Along with other important hormones such as prolactin, insulin and cortisol (stress hormone) your milk making factory is working hard in the subsequent phase of milk production called lactogenesis II. However, your milk will not ‘magically’ appear in large amounts after birth. Early hours or days after birth, you may notice little breastmilk which is yellowish gold in colour. That is the colostrum which is rich in antibodies and vitamin A. Gradually the amount of breast milk will increase and it may take 2-4 days before your milk starts ‘to come in’. If you are a first time mother, it may happen slightly later. Few days after birth, your breasts may start to feel ‘full’, which is a sign that your milk is coming in.
Whether or not you are breastfeeding during this stage, lactogenesis I and II will still take place as these two mechanisms are controlled by hormones. Some mothers have doubts that their body is not producing milk during the first few days after birth and therefore resort to alternatives such as formula milk. However, research has shown that mothers who breastfeed early and often during the first few days after birth (or express milk if baby is being separated) will make more milk later, and their babies will have less jaundice. If milk is not being effectively removed during this period, even by interfering with a breastfeeding session with only one bottle of formula milk, your milk production process will start to shut down.
Lactogenesis III
This is the maintenance stage of ‘mature’ milk production. It usually happens from around day 9 after birth, until the mother or baby decides to wean or stop breastfeeding. It is based on autocrine or local control, less by hormones. In this stage, milk production is mainly controlled by the breast, so the rate of milk production is mainly controlled by milk removal. As long as the milk is being drained or removed, the breasts will continue to make more milk. Therefore, it is very crucial for the mothers to always empty their breast by frequently breastfeeding their babies or pumping their milk in order to ensure adequate supply of breast milk.
Stomach capacity of Newborn

Pic source: Belly Bump
When the baby is born, the normal (physiologic) stomach capacity is estimated to be only about 7 ml which equal the size of a marble! Day by day this stomach capacity will increase. The amount of a mother’s colostrum is well matched to her baby’s stomach capacity. That is why mothers might notice the frequent feedings needed to feed the baby. Supplementing with formula milk can overfeed your baby causing them to have indigestion, frequent spitting or vomiting and being gassy.
Infant feeding cues
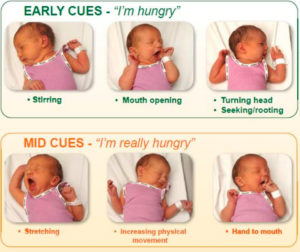 The most natural way to feed your baby is to feed him or her on demand. This means, that, the baby is fed whenever he or she shows any signs of hunger or feeding cues. The most obvious feeding cue would undeniably be crying, however, crying is actually a late hunger signal. Do not wait until your baby cries to be fed as this can cause stress in both the mother and baby and could result in feeding problems too. Therefore it is crucial that every mother is aware of these early subtle signs before the baby begins to cry for feeds. Infant feeding cues can be divided into early, active and late signs.
The most natural way to feed your baby is to feed him or her on demand. This means, that, the baby is fed whenever he or she shows any signs of hunger or feeding cues. The most obvious feeding cue would undeniably be crying, however, crying is actually a late hunger signal. Do not wait until your baby cries to be fed as this can cause stress in both the mother and baby and could result in feeding problems too. Therefore it is crucial that every mother is aware of these early subtle signs before the baby begins to cry for feeds. Infant feeding cues can be divided into early, active and late signs.
Early feeding cues include:
- Mouth opening
- Turning head, seeking or rooting
- Licking lips, smacking
Active hunger cues include:
- Fidgeting or stretching
- Fussiness
- Rooting towards the breast or around the chest
- Mouthing-sucking on lips, tongue, fingers or toes
Late signs (you may need to calm your baby prior to feeding):
- Crying
- Moving head from side to side
It is also good to know the risk factors for delayed onset of lactation. Delayed onset of lactation happens when the milk is very slow to come in or does not increase in volume as expected within three days after birth. However, just because your milk comes in late, it does not necessarily mean that you have no breast milk or low milk supply. There are many risk factors towards this delay, other than being a first time mother. Other factors include Caesarian section, prolonged second stage, pain medications during labour, retained placenta and high amount of blood loss. Since lactogenesis II is very much dependent on hormones, that means any maternal health issues that may interfere with the production or metabolism of hormones, such as type 1 diabetes, hypothyroidism and polycystic ovarian syndrome may result in delayed onset of lactation. In addition, structural breast abnormalities such as hypoplasia (underdeveloped breast), abnormal nipple anatomy such as inverted nipples may also interfere with the milk production and transfer.
So what am I going to do if my milk still does not come in by Day 3 or longer?
First of all, do not worry. Excessive stress may indirectly affect milk supply as it can interfere with your let down. If you find yourself in this situation, getting support and help from lactation consultant or counsellor is recommended, the sooner the better. The most important initial management is to optimize breastfeeding management, that is, to ensure that the breast is frequently and thoroughly emptied to ensure continuous milk production. Holding your baby in skin to skin contact and latching your baby as often as possible (or milk expression) will promote the hormones involved in milk production. To ensure that your baby is getting enough milk, monitor your baby’s weight as well as their dirty and wet diapers. Typically, expect one dirty diaper for each day of life (one on Day 1, two on Day 2 etc..) and one wet diaper for each day of life (one on Day 1, two on Day 2 etc..). Another indicator of adequate mother’s milk intake is the transition from the first dark stools passed by the baby to yellow stools by Day 5 and three to four stools per day by the fourth day of life.
In conclusion, all mothers can breastfeed their child unless they have certain medical conditions which need to be seen by a lactation consultant. There is no need to top up feeding with formula milk when the milk production or milk making process is understood. Happy breastfeeding to all mothers!
This article was written by
Dr Puteri Shanaz Jahn Kassim MD (USM) M.Med (Fam Med) IBCLC
Dr Nurjasmine Aida Jamani MD (UKM) M.Med (Fam Med) IBCLC
[This article belongs to The Malaysian Medical Gazette. Any republication (online or offline) without written permission from The Malaysian Medical Gazette is prohibited.]
