ASSUNTA HOSPITAL SERIES
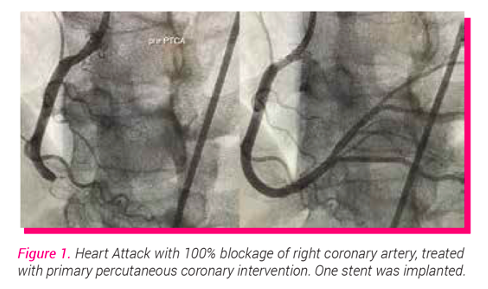
The paradigm shift of younger people presenting with heart attacks to the hospitals are evident now. Just a week ago, we activated the cardiac catheterisation laboratory (cathlab) for an emergency life-saving procedure called primary percutaneous coronary intervention (PCI) for a relatively healthy 40-year-old lady who had a heart attack. Her right coronary artery was 100% occluded and we were able to restore flow after ballooning and placing a drug eluting stent (see figure 1). She was discharged well after a few days. Coronary artery disease (CAD) is the leading cause of death in Malaysia and globally. The average age of Malaysians getting a heart attack is about 58 years and this is around 10 years premature compared to our Western counterparts.
Ischaemic heart disease (IHD) or coronary artery disease (CAD) occurs from a combination of several factors; mainly lifestyle, environmental influences, medical co-morbidities and genetic factors. Obesity and sedentary lifestyle are known contributing factors to IHD. In Malaysia, due the hot weather climate with the intermittent rainy weather, we tend to have less outdoor activities and sports. As for dietary influences, we are spoilt for choice. We have easy and cheap access to delicious Malay, Chinese, Indian and Western cuisines. Some of these nasi lemak (coconut fragrant rice with sambal), chicken rice, hokkien mee, curries and fast food have too much sugar, salt, oil, coconut oil, fat and food preservatives. The rich culture of Malaysia and up-bringing makes it tougher for us to cut down on these readily available food.
Genetic factors also play a role in coronary endothelial dysfunction and subsequent progressive atherosclerosis. Common genetic disease would be homogenous and heterogenous familial
hypercholesterolaemia (FH). Traditional non-modifiable cardiovascular risk factors are advance age, male, genetic history and family history. Meanwhile, modifiable risk factors are hypertension, diabetes mellitus, dyslipidaemia, abdominal obesity, tobacco smoking, trans fat and western pattern diet. A family history of premature coronary artery disease or heart attack is also a known risk factor.
Atherosclerosis begin as early as childhood and in post-mortem studies, little steaks of cholesterol plaques can be seen in the large arteries in the body such as the aorta. Atherosclerosis is the gradual process of cholesterol and inflammatory cell infiltration into the wall of the arteries, leading to progressive build of plaque. As age progresses, these cholesterol plaques can cause the vessels (arteries) to narrow, thus reducing blood supply to a particular organ such as the heart and brain, leading to heart attacks and strokes, respectively. With respect to this, it is alarming that we encounter many young patients below the age of 30 with high cholesterol.
Early features of narrowing of the heart vessels (coronary arteries) may include symptoms such as chest pain, chest discomfort and even shortness of breath. Many a times, this is activity related, such as walking up an incline or going up the stairs. Occasionally these symptoms will also disappear with rest after the brief period of exertion. Medically, this is termed stable angina or angina equivalent.
Annual cardiac health screening is strongly recommended as it is able to detect any symptoms and tailor appropriate investigations. Simple blood tests are able to detect risk factors such as high cholesterol, diabetes and pre-diabetes and assessment of other organs. Additional simple immensely useful tests are blood pressure reading and anthropometry measurements of height and weight; as they are able to provide body mass index (BMI) information and assessment for hypertension. Most people are unaware that early check-up even at the young age of 30’s is required if there is family history of high-risk cardiovascular diseases.
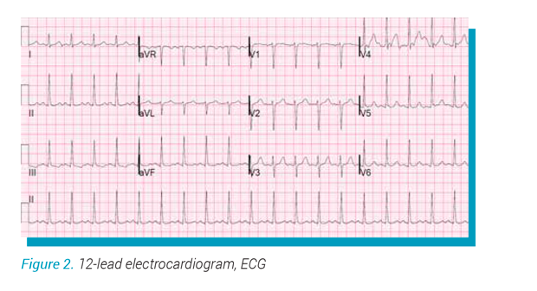
12-lead electrocardiogram (ECG) is a means to measure the electrical pattern of the heart via limb and
chest electrodes (see figure 2). This provides immense information during acute chest pain, especially in aiding the diagnosis of myocardial infarction (heart attack). In the clinic setting, ECG provides information of the conduction, rate, and any old heart attack traces.
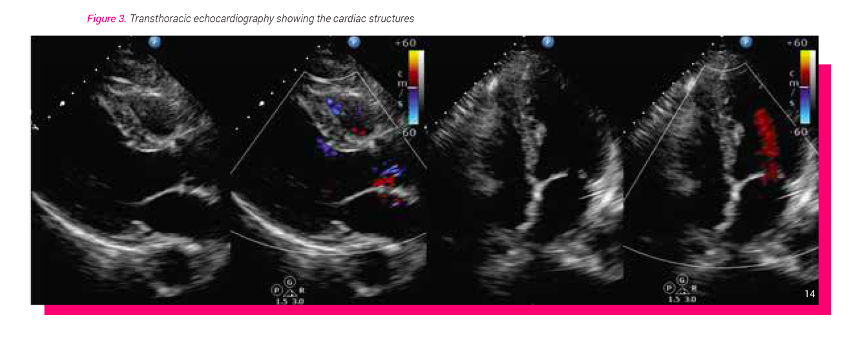
Echocardiography (echo) is a relatively quick ultrasound test to visualise the myocardium (heart muscle), heart chambers, heart valves and pericardium (see figure 3). By assessing the myocardial left ventricular systolic function will provide information about any possible underlying heart muscle disease and even coronary artery disease when there is territorial regional wall motion abnormalities (RWMA).
Exercise stress test is another simple cardiac screening method utilising the means of walking and jogging on a thread-mill while simultaneously monitoring for any symptoms, drop in blood pressure and abnormal changes or rhythm on ECG. In some individuals, running may be difficult on a treadmill, commonly due to any hip or knee problems. In this case, a dobutamine stress echo (DSE) may be preferred instead. Dobutamine is a pharmacological agent that is administered intravenously to stimulate the heart to beat faster. This in essence simulates a stressful environment for the heart and subsequent assessment may provide information regarding underlying coronary artery disease.
Another sub-speciality field that has developed immensely over the recent years is cardiac magnetic resonance (CMR). In addition to detecting heart muscle disease (cardiomyopathy), CMR is able to provide additional information if a particular area of myocardium is deprived of blood supply or unhealthy (scarred).
Calcium scoring is a means of utilising computed tomography (CT) scan to detect and quantify the presence of calcium of the heart vessels (coronary arteries). CT coronary angiography is a test frequently coupled together with calcium scoring. If the calcium score is not excessively high, intravenous contrast (dye) is injected and this helps to opacify (visualise) the coronary artery vessels during the CT scan. Subsequent 3D image reconstruction enables assessment of the degree of narrowing of the vessels.
In conclusion, as the saying goes prevention is definitely better than cure. Adding to that, early detection will enable better risk reduction and potential treatment of any severe cardiac disease.
Written by,
Dr Nicholas Chua Yul Chye
MBBS (Manipal) (Distinction), MRCP (UK),
Fellowship in Interventional Cardiology
(Barts Heart Centre, London)
Consultant Cardiologist

This is a sponsored post from Assunta Hospital (www.assunta.com.my) as part of an educational series of posts written by their healthcare professionals. For any enquiries regarding the services or treatment options provided kindly contact enquiries@assunta.com.my.
