Source: www.imt.ie
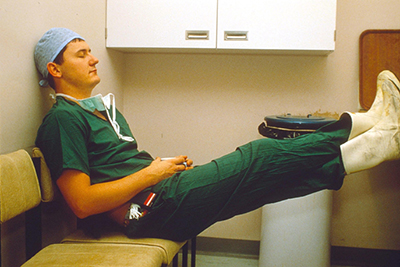
Working conditions, particularly long working hours, have always attracted significant discussion within the medical profession. More attention was drawn to this topic earlier this year when a medical officer was killed in a road accident after being on-call. Much of this discussion is typically based around personal and anecdotal experience. But what does the research literature say about working patterns of doctors influencing patient outcomes? And what impact does it have on doctors’ health?
We can debate about which work system (On-call vs Flexi vs other) is better or more detrimental; but, we need to understand the underlying concern should be how these systems contribute to fatigue. Even one-time exposure to a long or on-call shift impairs the cognitive and motor functioning of doctors1. In fact, cognitive performance after 24 hours of continuous wakefulness is akin to having a blood alcohol concentration of 100mg/dL2, twice the Malaysian drink driving limit. Therefore, systems that lead to sleep deprivation, prolonged wakefulness, enforced unnatural circadian rhythms and lack of recovery time all contribute to fatigue, and should be minimised or avoided.
Given the role of fatigue in doctors, it is not surprising that a review of 54 interventions3 to reduce residents working hours found beneficial outcomes in 73% of studies, including reporting fewer mistakes, percutaneous injuries and traffic accidents. However, some believe shorter shift lengths and fewer weekly work hours may compromise patient safety. This is evident from a SCHOMOS survey4 where only 22% felt the new Flexi-System gave House Officers more clinical exposure than the previous system; and 40% felt the new shift system provided continuity of care for patients.
Despite these concerns, there is little evidence to support this assertion. A review5 of 72 American and European studies found that reducing doctor working hours from more than 80 hours a week did not adversely affect patient safety and had limited influence on postgraduate training. It is worth noting that the same review could not conclude the effect of reducing working hours to less than 56 or 48 hours a week.
So while it is fair to say there is an absence of clear beneficial evidence for reducing doctor working hours, this statement ignores the findings that there is, equally, no clear detrimental impact on patient and training outcomes. Perhaps, an additional question worth considering is: what impact do these reduced hours have on the safety and health of doctors themselves?
In response to the aforementioned traffic incident, a survey6 of 430 doctors who had been involved in a road accident post-call observed that 60.2% of accidents occurred after being on duty for more than 24 hours, and that 25% of accidents resulted in some form of injury or death. This is consistent with international findings that doctors working a 24 hour or longer shift were more than twice more likely to be involved in a road accident than those on a standard shift7-8. Residents who were on call every fourth or fifth night have similar attention, vigilance and simulated driving performance to the drink driving limit9. These findings echo many anecdotal experiences, highlighting fatigue and fatigue-related cognitive impairment as significant risks to doctors’ (and other road-users’) safety.
Further systematic reviews have observed shorter shift lengths10 and fewer weekly work hours3,11 to be associated with enhanced safety and health among doctors; with approximately two third of studies demonstrating such a link. In addition to motor vehicle accidents, the link between working patterns and percutaneous injuries is fairly well established.
The broad trend of relationships indicate that long working hours and shift work is associated with poorer doctor health, including general wellbeing, mood disorders and burnout, although this evidence is less conclusive than it is with safety behaviours. This is partially due to the complex nature of occupational wellbeing which is not reliant on work patterns alone.
Within the Malaysian context, lower emotional burnout was observed in residents who worked for less than 60 hours (instead of 72 hours)12, were satisfied with the implementation of the new Flexi-System and perceived less role overload13. Long working hours are linked with high workloads, mentally demanding work, and work-family conflict, all of which have been identified as significant sources of stress amongst Malaysian medical officers14-15. Medical officers exposed to such working conditions also had normal and abnormal anxiety that were nine times higher than their counterparts in less challenging work environments16.
In conclusion, the evidence that fewer working hours and better shift structures results in beneficial patient outcomes is not conclusive, although general trends lend some support to this hypothesis. This should not distract from focusing on what effect long working hours and shift work has on the safety and health of doctors. Rather than strive towards a pre-set number of working hours or a particular shift pattern, changes to working patterns should emphasise reducing fatigue of doctors. We also have to recognise that this constitutes only part of the wider picture. Changes need to coincide with appropriate support in other aspects of the working environment, including: safe staffing levels, adequate resources, safe handovers and proper supervision.
Kevin Teoh is a PhD candidate with the Dept. of Organizational Psychology, and a research assistant at the Centre for Sustainable Working Life at Birkbeck, University of London.
Dr Juliet Hassard is an Occupational Health Psychologist and Deputy Director at the Centre for Sustainable Working Life, Birkbeck, University of London.
Dr Chua Li-Shun is a Medical Officer at Hospital Sungai Buloh and also an editor for the Malaysian Medical Gazette.
References
- 1Flinn F, Armstrong C. Junior doctors’ extended work hours and the effects on their performance: The Irish case. International Journal for Quality in Health Care, 2011; 23(2):210-217.
- 2Dawson D, Zee P. Work hours and reducing fatigue-related risk: Good research vs good policy. JAMA, 2005; 294(9):1104-1106.
- 3Fletcher KE, Underwood III W, Davis SQ, et al. Effects of work hour reduction on residents’ lives: A systematic review. JAMA, 2005; 294(9):1088-1100.
- 4Selvadurai TK. Review of the houseman’s Flexi Hour Shift System. Berita MMA, 2012; 42(7):14-16.
- 5Moonesinghe SR, Lowery J, Shahi N, et al. Impact of reduction in working hours for doctors in training on postgraduate medical education and patients’ outcomes: Systematic review. BMJ, 2011; 342:d1580.
- 6Islamic Medical Association of Malaysia. Post-call MVA Survey, 15 July 2015. Available at: http://imamalaysia.org/wp/?p=796
- 7Barger LK, Cade BE, Ayas NT, et al. Harvard Work Hours, Health, and Safety Group. Extended work shifts and the risk of motor vehicle crashes among interns. New England Journal of Medicine, 2005; 352:125-34.
- 8Parthasarathy S, Hettiger K, Budhiraja R, et al. Sleep and well-being of ICU housestaff. Chest, 2007; 131:1685-93.
- 9Arnedt JT, Owens J, Crouch M, Stahl J, Carskadon MA. Neurobehavioral performance of residents after heavy night call vs after alcohol ingestion. JAMA, 2005; 294:1025–1033
- 10Reed DA, Fletcher KE, Arora VM. Systematic review: Association of shift length, protected sleep time and night float with patient care, residents’ health, and education. Annals of Internal Medicine, 2010; 153(12):829-842.
- 11Rodriguez-Jareño MC, Demou E, Vargas-Prada SV, et al. European Working Time Directive and doctors’ health: A systematic review of the available epidemiological evidence. BMJ Open, 2014; 4:e004916 .
- 12Al-Dubai SAR, Ganasegeran K, Perianayagam W, Rampal KG. Emotional burnout, perceived sources of job stress, professional fulfillment, and engagement among medical residents in Malaysia. The Scientific World Journal. 2013; 9.
- 13Aminah A. Work-family conflict among junior physicians: Its’ mediating role in the relationship between role overload and emotional exhaustion. Journal of Social Sciences. 2010; 6(2):265–271.
- 14Razak, A.Z.A.A., Yunos, N.K.Y, Nasurdin, A.M., 2011. The impact of work overload and job involvement on work-family conflict among Malaysian doctors. Labuan e-Journal of Muamalat and Society, 5 1-10.
- 15Yusoff, M.S.B., Esa, A.B., 2011a. Stress, stressors and coping strategies among house officers in a Malaysian Hospital. ASEAN Journal of Psychiatry, 12 (1), 85-94
- Tan, S.M.K., Jong, S.C., Chan, L.F., Shah, S.A., 2013. Physician, heal thyself: The paradox of anxiety amongst house officers and work in a teaching hospital. Asia-Pacific Psychiatry, 5 (S1) 74-81.
[This article belongs to The Malaysian Medical Gazette. Any republication (online or offline) without written permission from The Malaysian Medical Gazette is prohibited.]
