The liver has an amazing capacity to heal and regenerate. Is a fact, which is often negated when the liver is healthy, carrying out its functions without complaint. With thousands of chemical and toxins passing through the liver each day, depending on what we consume, our liver never gives up on us – ensuring that our health is kept in check and balance.
The problems kick in when the liver stops functioning whenever certain infections or chemicals overwhelm its capabilities. Few of us notice the yellowing of the skin and the eyes when this happens. This is termed jaundice and it is one of the earliest symptoms of acute liver failure. Subsequently the person would become excessively tired and, if left untreated, they can progress to other symptoms like easy bruising and bleeding. It is no surprise that doctors equate the human liver to that of a car’s engine. Without it, the body’s functions are not able to be executed with precision.
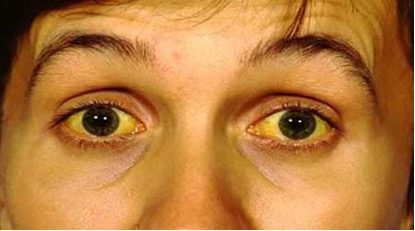
Figure 1: Yellowing of the skin and eyes is termed jaundice – the old term is icterus (courtesy of http://www.ahealthdiary.com)
Despite the vast amount of research put into identifying each chemical that we take in day in and day out, we can never keep up with the ever-increasing number of new drugs that are out there in the market. We certainly do know what medications can lead to liver injury, but the truth is that we can never know everything. Therefore, doctors would not be able to give you a definite answer as to whether a certain slimming product, those wonderful antioxidants or that cleansing tea would be safe for you.
A scarred liver is called liver fibrosis in medical terms. As it progresses, it becomes cirrhotic (a more advance state of fibrosis), a condition that carries the risk of developing hepatocellular carcinoma (liver cancer). Fibrosis means thickening of tissue, for example scarring of the skin. Imagine that happening in your liver. Despite its enormous ability to repair itself, ongoing insults on the liver would eventually overwhelm its reparative efforts and scar tissue will form. If you have ever seen a liver specimen, for example in the wet market, you will instantly notice how smooth the surface looks like. Picking one up and feeling the texture would give you an idea of how pliable it is, its firmness and its ability to bounce back to its normal state when pressed.
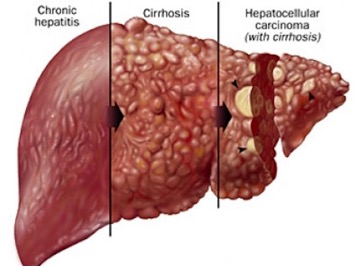
Figure 2: From ongoing inflammation (chronic hepatitis) to cirrhosis (advanced state of fibrosis) to hepatocellular carcinoma (liver cancer as a complication; courtesy of http://uct-clinic.com)
The same applies to the human liver. Should fibrous tissue start replacing the normal liver tissue, this would eventually lead to a hardened liver. Some common causes of liver fibrosis/cirrhosis are as follows:
- Viral hepatitis – Hepatitis B and C infection
- Alcohol
- Non-alcoholic fatty liver disease
- Autoimmune hepatitis
- Primary biliary cirrhosis
- Primary sclerosing cholangitis
- Drugs and toxins
- Wilson’s disease
Autoimmune hepatitis occurs when stray antibodies becomes confused and start to injure the host liver’s tissues, which then leads to ongoing inflammation and subsequently scarring. In primary biliary cirrhosis and primary sclerosing cholangitis, these antibodies are directed against the bile ducts of the liver and subsequently the liver tissues themselves. These are rare conditions. The commonest cause, which is predicted to top the list in the coming decades, is fatty liver. This is because obesity is now so prevalent.
As liver cancer still has extremely grim outcomes, treatment is directed towards discovering the early stages of liver injuries and halting its progression. Not only would one live in constant fear of liver cancer, but also its associated complications like vomiting blood, swollen abdomen, infection, increased risk of other forms of bleeding and finally “liver coma”. The earliest detection of a scarred liver is often through blood investigations which reflect the liver enzymes (chemicals) but this may not always be accurate. If you are at risk of developing liver cirrhosis, you should get yourself seen by a doctor who will then explain things further.
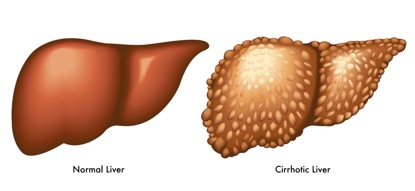
Figure 3: Comparison between a normal liver to a cirrhotic liver – notice the multiple rounded growth developing on the liver surface; these are irreversible fibrotic liver tissues (courtesy of www.bahola.co)
With modernisation of medical technology and the equipment available, we can now stage the severity of a scarred liver through non-invasive investigations that are programmed to measure how thick the scarred liver is. These are called Fibroscan or Shear Wave Elastography. Prior to this, the only way to tell the severity of scarring was through liver biopsy where a needle is guided by radio-imaging methods to obtain tissues from the liver. Categorising the stages of cirrhosis is important for doctors to determine timing of treatment especially for viral hepatitis.
The following is a summary of the above:
- Factors causing liver injury
- The reparative mechanism – most heal after the cause is addressed
- Ongoing liver injury results in persistent inflammation (hepatitis)
- Liver fibrosis sets in (scarring development)
- Cirrhosis develops over years of unidentified and untreated liver injury
- Risk of developing liver cancer escalates with cirrhosis
- Complications of cirrhosis
- Assessment of severity of cirrhosis to aid in treatment
Many patients want to know what scarring of the liver means and I hope this article has shed some light on how scarring of the liver happens and its complications.
Dr. Chiam Keng Hoong is an internal medicine physician and a MRCP holder. He currently works in Sabah.
[This article belongs to The Malaysian Medical Gazette. Any republication (online or offline) without written permission from The Malaysian Medical Gazette is prohibited.]
