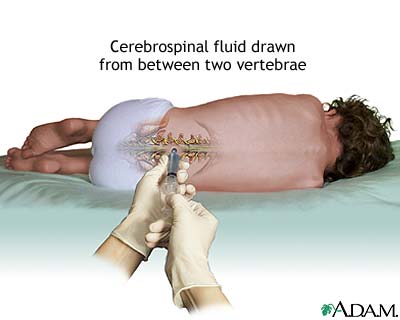
Source: A.D.A.M. Interactive Anatomy
Introduction
The above response is sometimes heard in local hospitals when a doctor attending to a child patient proposes to the parents or guardians to retrieve a sample of the spinal fluid. Although modernisation has penetrated certain aspects of our community, some perceptions remain difficult to change. Part of it is the procedure to collect sample of spinal fluid or lumbar puncture (LP). It is hoped that with this article, questions and confusions on the procedure will be clarified.
What is the spinal fluid?
Before we delve into the subject, let us look at the anatomy of the body involved.
The brain and the spinal cord are organs that are kept in a very close sequence. Both are coated in a membrane tissue called ‘meninges’. The brain is located intact within the skull. The spinal cord, a network of tissue that begins from the lower part of the brain and continues downwards towards the body, is protected by the back bones that are known as the vertebras. The back bone or the vertebrae is unique as it is not connected in a single tube like a pillar, instead it consists of smaller sections in a neat arrangement on top of one another. They are connected by a structure called the spinal disc, which plays a role to absorb impact during daily activities.
The brain and spinal cord are constantly saturated with a liquid known as the cerebrospinal fluid (CSF). The CSF is produced in the brain all the time. It goes through a channel from the brain into the spinal cord network. The fluid collected at the bottom of the spinal cord is reabsorbed and returned to the brain where the CSF production process starts. The function of CSF includes protecting the brain and the spinal cord from impact from the walls of the skulls and the hard vertebrae structure.
What is this procedure about?
The lumbar puncture procedure is a process to access the CSF or the space where the fluid is kept. Once this access is gained, various objectives can be met depending on the clinical situation being faced. As explained above, the brain and the spinal cord is kept in a very close sequence. It is very difficult for a doctor to make evaluation on the nervous system when a patient is suspected to have a related problem. The advantage of having access to the CSF or the space where the fluid is kept enables doctors to perform more detail evaluations and investigations so that a more accurate diagnosis can be made and the best treatment can be provided to the patient.
Why is this procedure done?
In children, one of the main indications to perform a lumbar puncture (LP) is when the child is suspected to have meningitis (acute inflammation of protective membranes covering the brain and spinal cord caused by infection or certain drugs). This is because other tests such as blood samples and brain scans will not be sufficient to achieve an accurate diagnosis.
On top of that, there are times when children who are having an infection of the brain may not show classical or regular signs and symptoms of the infection. This makes it challenging for doctors to make a diagnosis.
With the CSF, a detail analysis can be made so that the best and most accurate treatment can be provided. If this sample is not obtained, treatment will be based on readily available clinical evidence. However, the presence of organisms which caused the infection will not be able to be determined. Complications will arise if the child does not show a positive response towards early treatment and this will complicate the next step in treating the patient because there is no solid evidence to draw a plan for the patient’s treatment.
Lumbar puncture is also done to deliver medications or reduce intracranial pressure in selected cases.
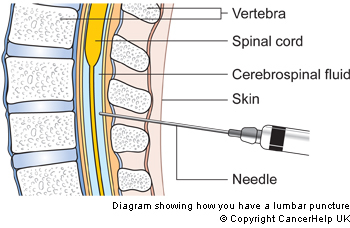
Source: www.cancerresearchuk.org
How is this procedure done?
This procedure usually takes between 20 to 30 minutes. Depending on the patient’s condition, anaesthetics may or may not be used. No specific preparation is required. The procedure is done in a sterile setting using a special needle.
Before that, a pain relieving cream will be applied to the skin surrounding the backbone area. Painkiller injections may be given depending on the clinical condition. The doctor will then choose a specific location for the lumbar puncture, which is between the vertebras and away from the spinal cord network. A needle is then inserted into the selected location. The cerebrospinal fluid sample is extracted out through the needle and collected into a tube for analysis. Only a few drops are required.
When it is done, the needle is taken out and the area is covered with a pressure dressing for a short while to ensure no bleeding or spinal fluid leakage.
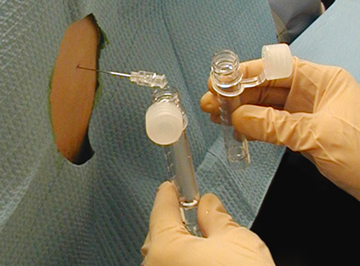
Source: www.diagnosisms.com
What are the possibilities of complications?
For children considered fit for LP, a possible complication that may arise is pain at the punctured area for a few hours. Some children experience headaches, but both conditions are temporary and patients will be advised to lie down or rest for a few hours and increase water intake.
Because the location where the needle is inserted is away from the spinal cord, there is no issue of causing the patient to be paralysed. The backbone or vertebrae will not be hurt in the process as the puncture is done in the space between the bones.
The spinal fluid taken will be replaced by the brain because the production of CSF is continuous.
Other possible complications are irritation or infection of the area where the needle was inserted. This rarely happens as the procedures are done under sterile method by trained doctors.
Is this procedure safe?
In cases that have been deemed suitable by the doctor in charge, the procedure is very safe. LP plays an important role in investigating illnesses related to the brain and spinal cord as well as certain other diseases. It is normal for parents to be worried when a doctor suggests the procedure. The staff involved should also be sensitive towards the parents’’ feelings. Both parents and doctors must be in mutual understanding so that any doubts and questions can be clarified.
Dr. Alya Hamzah is a paediatrican who is currently based in Sabah. She places high importance on educating patients and their families to ensure optimum treatment is provided. Find out more on The Team.
[This article belongs to The Malaysian Medical Gazette. Any republication (online or offline) without written permission from The Malaysian Medical Gazette is prohibited.]
References :
- http://www.childrenshospital.org/health-topics/procedures/spinal-tap-and-lumbar-puncture
- http://kidshealth.org/parent/general/sick/lumbar_puncture.html
