Source: penangsurgeon.com
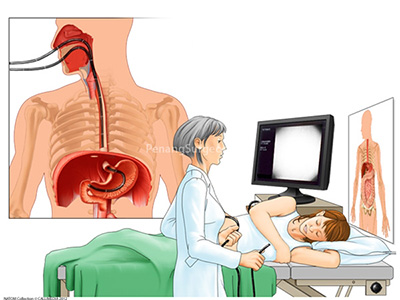
Having a tube down your throat is something people don’t take lightly. The nightmarish thought of inserting a long tube from the mouth down to the early portions of the small intestine is not only scary but utterly outrageous for some patients.
Patients often ask the degree of pain that they will have to endure, mostly from past experiences and encounters of friends or close relatives that regale them with vivid details of perhaps exaggerated imagery. I have failed miserably in getting patients to have an OGDS done purely because of the fact that they are too scared of the procedure despite having explained down to the last detail, showing them video presentation and even diagrams from my consultation room. Aside from pain, a handful would be worried of the side effects such as perforating their throat, bleeding from manipulation of the scope, introducing infection, as well as unable to withstand the bloated sensation due to air being pumped to inflate the stomach, in order to ease the operator for viewing the stomach and the small intestines.
Why Do You Need A Diagnostic OGDS?
- Unexplained low hemoglobin count/red blood cell (often done with colonoscopy)
- Stomach bleeding
- Dyspepsia (indigestion)
- Heartburn
- Acid reflux symptoms
- Persistent vomiting and/or nausea
- Difficulty in swallowing or painful swallowing
- Suspicion of symptoms of gastric cancer
- Surveillance of engorged or swollen blood vessels in conditions of chronic liver disease
NB: OGDS can also be therapeutic where interventional measures are carried out to stop bleeding, to sample biopsy and to band swollen and engorge vessels amongst other things.
The Preparation Prior to the OGDS Suite
The doctor in charge would preferably choose to either admit you a day before the procedure or put you under the day care option. You are not to take any solids or liquids for a specified duration prior to the procedure. You will need to sign a consent form stating that you have understood and agreed to the procedure.
The Preparation inside the OGDS Suite

Figure 1: An exploded image of a new OGDS machine – the upper panel reveals the live imagery of the OGDS procedure while it is being carried out while the lower panels are responsible for video recording, photography, printing and other ancillary scope functions.

Figure 2: A patient being prepped for OGDS in the center that I am working in. The older model is to the left of the picture with the black TV screen. The newer model is purely for experimental usage.
After briefly explaining the procedure to you again, the doctor or the nurse would then administer the lignocaine spray towards the back of your throat to numb it so that you would not encounter any pain. Regardless, you will still feel a slight pressure with the advancement of the scope into your throat and a reflexive regurgitation every once in awhile, which is common to all. The taste of the lignocaine spray can be bitter and you would be required to swallow it to numb the lower portions of the throat that could not be reached externally. Some patients have reported difficulty in breathing but these are short-lasting and could be reduced by taking deep slow breaths through your mouth. After half a minute to a minute, the nurse will put a mouthpiece which encircles the inner lining of your mouth. This is painless but is necessary to avoid you from biting down on the scope which is an expensive instrument. A small cylindrical tube would be inserted at the corner of your mouth after the mouthpiece has been inserted to drain out saliva and secretions throughout the procedure.

Figure 3: A flexible older generation OGDS (or also known as upper endoscope) on display in my center alongside intervention tools and other OGDS paraphernalia.
The Procedure
The operator (also known as the gastroenterologist or physician) will then start the procedure after lubricating the tip of the scope with a prescribed gel to ease manoeuvrability. He will try to minimise as much possible the contact with the surrounding throat and a swift attempt at intubation of the oesophagus (swallowing the tube) would be done. Sometimes the doctor will ask your cooperation to swallow and in which the scope would be driven deep into the oesophagus (during the swallowing process) with ease and without much difficulty. It is unusual, although it happens, that at this stage patient would develop a sensation of wanting to regurgitate and they sometimes do.
A thorough diagnostic OGDS can take anywhere between 5 to 10 minutes where the operator will look first at the oesophagus, then the stomach and the duodenum (the early portion of the small intestines) before flexing the scope back to look at the fundus of the stomach (which is the first part of the stomach). Photo shots will be taken and in some advance scopes, even videos can be taken. Biopsy would also be taken for further test to diagnose Helicobacter pylori before the scope is finally withdrawn. A great deal of pathology can be seen from the OGDS itself and these includes stomach or duodenal ulcers, bleeding ulcers, herniation of the oesophagus, malignant or benign growth, features to suggest ongoing acid reflux and swollen/engorged blood vessels in the oesophagus. As the scope advances, the operator would usually pump in air to inflate the stomach and the patient would often complain of a tolerable degree of abdominal discomfort. Prior to the completion of the procedure, the operator would suck out the air blown into the stomach to ease the symptoms.
Do keep in mind that should any intervention be required during the OGDS, the procedure can sometimes lasts up to 30 minutes or more depending on the complexities of the case. And if such things are anticipated, the doctors will often inform you beforehand.
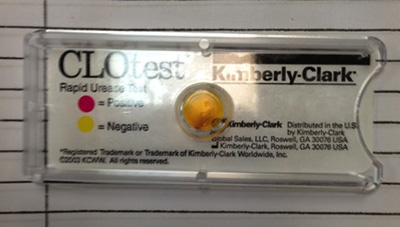
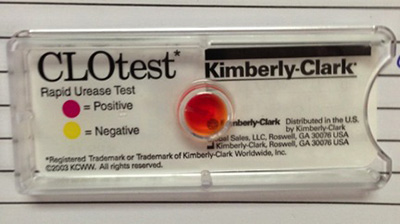
Figure 4: Pictures showing a rapid detection kit aptly named CLOtest manufactured by Kimberly-Clark for the Helicobacter pylori bacterium as the colour turns from yellow to red. The time taken to turn positive can be rather immediate depending on the severity of the infection, but it can take up to 30-60 minutes for the results to be conclusive.
Conclusion
If you have any questions regarding the procedure, you can direct your questions to the doctors who are in-charge of you and/or doctors who will be carrying out the scope.
Dr. Chiam Keng Hoong is an internal medicine physician and a MRCP holder. He currently works in Sabah.
[This article belongs to The Malaysian Medical Gazette. Any republication (online or offline) without written permission from The Malaysian Medical Gazette is prohibited.]
